
The vagus nerve is involved in nearly every physiological action in the human body and harnessing its power can have an immediate and dramatic impact on your well-being.
Metaphors abound for the vagus nerve:
- The superhighway of your body, transporting vital information between your brain and the rest of your internal organs;
- A symphony conductor, directing how fast or slow, loud or quiet your nervous system will be at any given time;
- Air traffic control, monitoring a multitude of moving parts to make sure all of the physiological airplanes fly safely and efficiently to their destination.
In a time when we all speak the universal language of hyperbole, it would be easy to dismiss this vagus talk as just another passing trend from a wellness culture that promotes and discards the next! big! thing! for sport. (Literally.)
But, here’s the deal. Physicians as far back as the Roman Empire1 have been grappling with how the vagus nerve impacts bodily function. We’ve now learned that simple movement and breath exercises can be done at home to manually stimulate the vagus nerve in times of stress to trigger the body’s natural relaxation response. And for patients with conditions ranging from epilepsy to rheumatoid arthritis to Crohn’s disease, electronic vagus nerve stimulation is offering hope and showing long-term results. The power of the vagus nerve lies in its ability to impact physical and emotional conditions that have proven to be difficult to treat with traditional drug and medical interventions. When people run out of options—for medical disorders or stress management— they find their way to the vagus, and realize the power this one part of our anatomy has over the entire system.
The hype is now consensus; the future of medicine and self-care will be interwoven with our understanding of the vagus nerve and how it works.
But First, What is the Vagus Nerve?
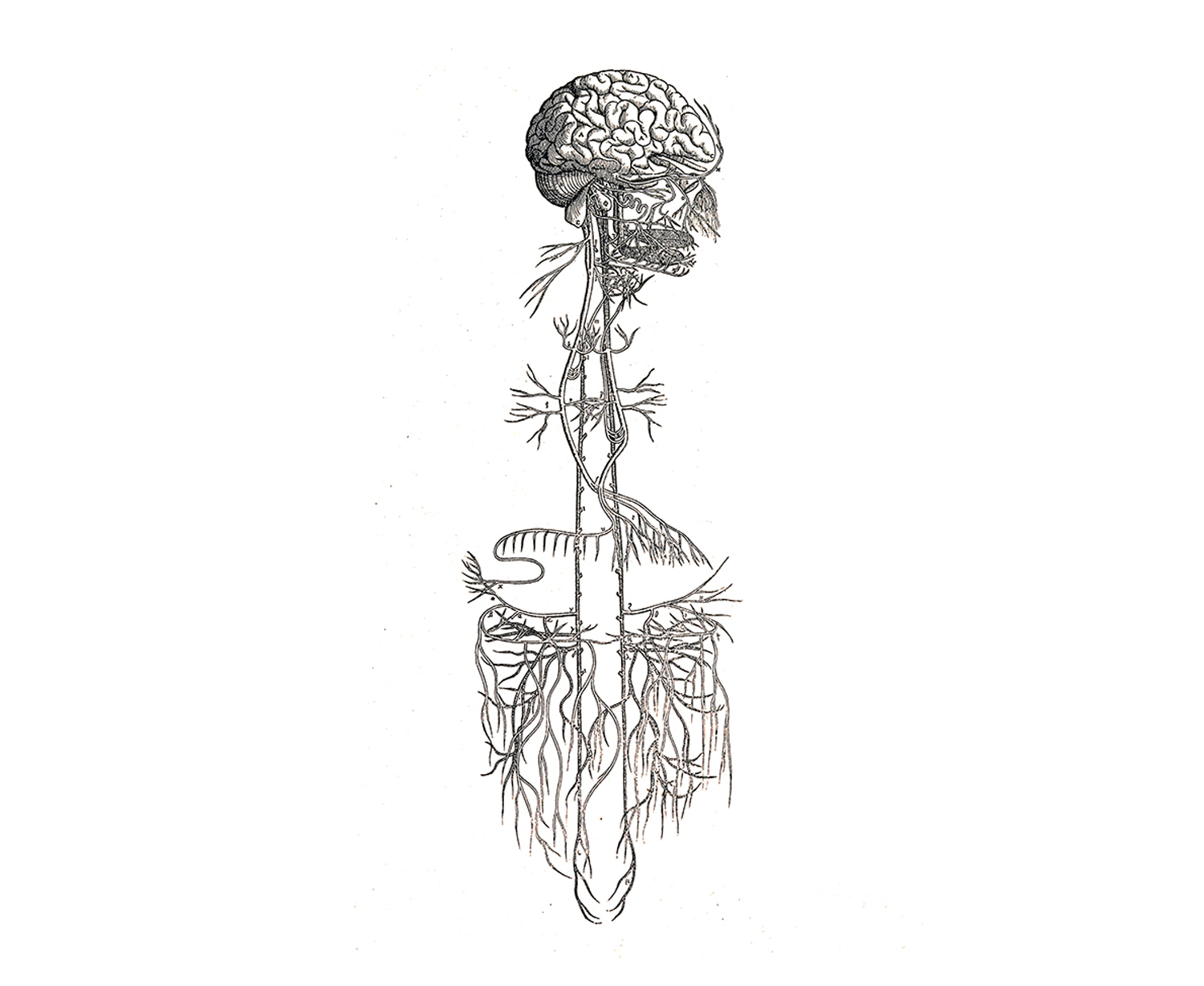
The vagus is the tenth cranial nerve, originating in the brain stem and traveling through the face, neck, lungs, heart, diaphragm and abdomen, including the stomach, spleen, intestines, colon, liver, and kidneys.2 Vagus is Latin for “wanderer,” an appropriate name for the longest cranial nerve in the body. The vagus nerve is intricately connected to mood, immune response, digestion, and heart rate.3
Why is everyone talking about the vagus nerve right now?
Maybe you know a little bit about the vagus already, or perhaps you’re reading about it for the first time. Now that it’s on your radar, you’ll start to notice it everywhere, from podcasts to Facebook groups to mainstream news articles. Marriage and Family Therapist Justin Sunseri launched The Polyvagal Podcast, a show about all things vagus nerve, in February of 2019 and quickly built an audience of thousands each month alongside his co-host Mercedes Corona. “I felt a compulsion to do it,” says Sunseri. “I literally woke up one night at four in the morning and the words Polyvagal Podcast were pounding in my head. I knew the information would be really good, but I had no idea what the bigger picture would be.”
Lisa Elliott is an aerial acrobat in Seattle who discovered the vagus nerve after a near-death experience from an aortic dissection. She started the Vagus Nerve Study Group in her living room with six friends in 2015, and it’s morphed into a thriving Facebook community with almost nine thousand members studying the vagus together. “When I first started studying it, I was interested in the vagus nerve as a discrete anatomical structure,” says Elliott. “What is this thing that can make a big difference in chronic illnesses? But over the years, I came to see it as an anatomical map that can lead us to a new way of thinking about our bodies and beings, our emotions, and our interaction with the environment.”
Electronic Vagus Nerve Stimulation (VNS)
On the medical front, Dr. Kevin Tracey is a neurosurgeon who has done groundbreaking work in the field of bioelectrics, where a small electronic device is implanted under the skin of a patient’s chest to send electrical impulses to the vagus. He published a study in 20024 about mice with strokes, revealing that vagus nerve stimulation turned off the body’s production of tumor necrosis factor (TNF), a molecule produced by the immune system during an inflammatory response that, when regulated, is good for the body, but in excess can damage organs, cause blood pressure to drop, and lead to septic shock.5 This prompted a clinical trial using VNS on rheumatoid arthritis patients6 with high levels of TNF that caused debilitating pain. At the end of the forty-two day study, the TNF levels of study participants were nearly the same as non-arthritic patients. Their pain was almost gone, joint swelling was reduced, and mobility had returned. Dr. Tracey has also had success with Crohn’s disease patients, and sees a future when diseases like Alzheimer’s, cancer, diabetes, and hypertension can be treated with bioelectronics. VNS has been approved by the FDA to treat epilepsy since 1997, and depression since 2005, but everything else right now is in the clinical trial stages. In addition to Dr. Tracey’s work, there are studies being done on the impact of VNS on diabetes, stroke recovery, glucose metabolism, and many others around the world.
While researchers and the medical establishment wade through lengthy clinical trials and FDA approval processes, the good news is that it doesn’t require a surgical implant to impact your vagus nerve.
Manual Stimulation of the Vagus Nerve
Physical therapist and functional manual therapist Gregg Johnson uses his hands to do manual work on the vagus, and trains other practitioners to do the same at his Institute of Physical Art in Colorado. He’s been a physical therapist for fifty years, but stumbled into an interest in the vagus nerve five years ago when he had a student who had high blood pressure and an elevated heart rate, and was looking for a way to avoid going on long-term medication. Johnson palpated (examined with his hands) the neck, and could feel that the vagus nerve was in tension. “This was the first time I had selectively, consciously palpated the vagus nerve,” says Johnson. “All of the sudden, as everything started enhancing in mobility, his heart rate normalized and he started feeling like he hadn’t for months. And that night when he tested his blood pressure it had returned to normal.” Since then, Johnson has used manual vagus nerve stimulation to help patients with irritable bowel syndrome, kidney problems, and fertility issues, just to name a few.
JARGON ALERT
Palpate: to examine a part of the body by touch for medical purposes
This myofascial self massage shows both manual hand and soft-tool palpation.
There are a number of things you can do with breath and movement on your own at home to manually stimulate the vagus nerve. But to understand how, first it helps to understand a little bit more about the anatomy and function of the vagus nerve itself.
Vagus Nerve Function
The vagus nerve is part of the autonomic nervous system, the body’s unconscious control system that helps regulate our internal organs to optimize health, growth, and restoration, a concept known as homeostasis.7 The autonomic nervous system is divided into two branches— the sympathetic branch, which mobilizes you for action (the “on” switch); and the parasympathetic branch, often referred to as the rest-and-digest state (the “off” switch). The vagus nerve resides in the parasympathetic branch of the autonomic nervous system. Much of our understanding of how the vagus functions within the parasympathetic branch, and our ability to impact it through breath and movement, can be traced to Dr. Stephen Porges and the introduction of his Polyvagal Theory in 1994.
JARGON ALERT
Autonomic Nervous System: the part of the nervous system that unconsciously controls bodily function, including things like heart rate, breathing, and digestion. There are two branches of the Autonomic Nervous System:
- Sympathetic: your body’s ON switch, supporting mobilization for action
- Parasympathetic: your body’s OFF switch, supporting relaxation
The Polyvagal Theory
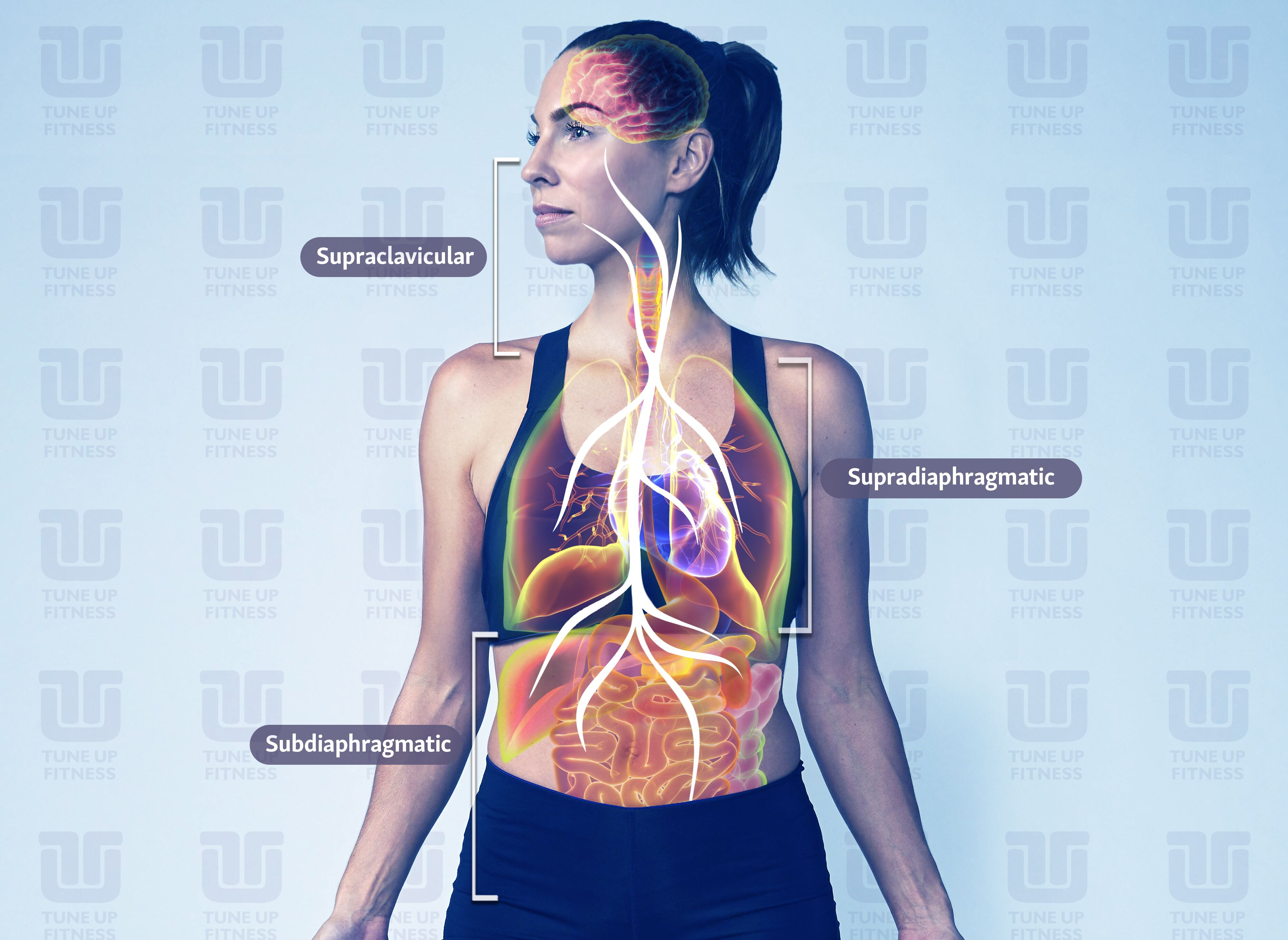
The Dorsal Complex and Shutdown
Dr. Porges identified two pathways of the vagus nerve. The first pathway, the dorsal complex, is left over from our pre-mammalian, ancient vertebrate ancestors. It’s often called the sub-diaphragmatic branch of the vagus, because it originates in the brain stem and supplies nerves to the visceral organs below the diaphragm, including the stomach, liver, spleen, kidneys, gallbladder, urinary bladder, small intestine, pancreas, and ascending and transverse parts of the colon.8 It’s unmyelinated, which means it lacks a myelin (fatty) sheath, and consequently transmits information slower than a nerve that’s myelinated. When humans or other mammals sense they are in grave danger, a surge in dorsal activity can result in system shutdown, including a drop in blood pressure, with a potential for fainting or state of shock.9 The dorsal vagal response is referred to in shorthand as shutdown.
The Ventral Complex and Safety
The second pathway of the vagus nerve is the ventral complex. It formed as we evolved from ancient reptiles to mammals, and originates in the brain stem in the nucleus ambiguus, a group of motor neurons connected to the muscles integral to speech and swallowing, such as the soft palate, pharynx, and larynx.10 The ventral vagus is the primary regulator of the heart rate, and muscles in the face and head. This newer ventral vagal path is myelinated and transmits information much faster than the dorsal vagal path. It’s what’s commonly referred to as our safe and social state, and evolved to provide a social engagement system, which was necessary in order for mammals to coexist, work in community, and reproduce. People in a ventral vagal state are generally engaged in the world, and open to connecting and cooperating with others.
Between the development of the dorsal vagal path and ventral vagal path, the sympathetic branch of the nervous system formed, allowing for mobilization in times of stress. This is most often referred to as the fight-or-flight reaction.
JARGON ALERT
Dorsal Vagus: The oldest part of the vagal complex, left over from our pre-mammalian ancient vertebrate ancestors. A dominant dorsal vagus results in a shutdown state.
Ventral Vagus: The newest part of the vagal complex, developed during our evolution from reptiles to mammals. A dominant ventral vagus presents as a feeling of safety and social engagement.
Sympathetic: This part of the nervous system developed between the Dorsal and Ventral vagal complexes; supports mobilization by increasing blood flow throughout the body.
Polyvagal Theory
Polyvagal Theory identifies how these three neural (of or relating to nerves or the nervous system) circuits— the dorsal vagal, sympathetic, and ventral vagal— are involved in evaluating our environment and reacting to cues of safety or threat. There are three organizing principles of the polyvagal theory11:
-
Hierarchy
The autonomic nervous system responds to cues in the environment in a specified and predictable way. Either in order from the oldest to newest neural circuits (dorsal, sympathetic, ventral), or the newest to oldest (ventral, sympathetic, dorsal).
-
Neuroception
This is a concept coined by Dr. Porges, and describes how our autonomic nervous system subconsciously evaluates and responds to cues of safety or danger in our environment. “Detection without awareness,” Dr. Porges says. The vagus has more than 100,000 nerve fibers, and communicates bidirectionally between the brain and the body, with 80% of the fibers communicating from the body to the brain, and the other 20% communicating from the brain to the body.12 So, that “gut feeling” you’ve felt before— that’s neuroception. It’s your body having what amounts to a “sixth sense” moment, and communicating that information to your brain.
-
Co-regulation
This is the mutual regulation of physiological state between individuals.13 One example Dr. Porges uses for co-regulation is the relationship between a mother and her baby. If a mother is calming her child and the child responds by relaxing and vocalizing sounds of contentment, this has a reciprocal effect of calming the mother. If the infant continues to be upset and doesn’t respond to the mother’s attempt to settle her, the mother will also get upset. Dr. Porges calls this our “biological need to connect.”
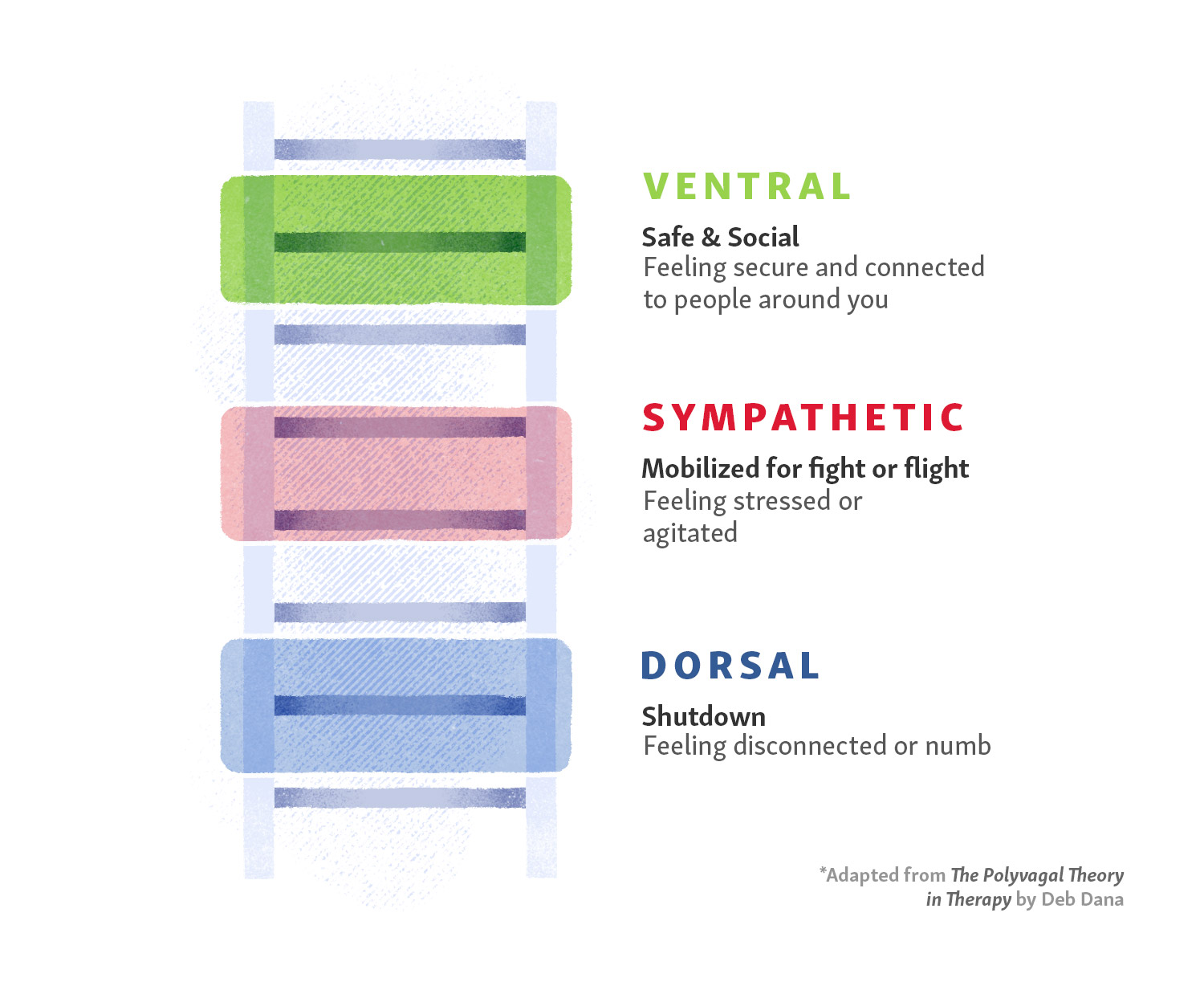
The Polyvagal Ladder
Deb Dana, author of the book The Polyvagal Theory in Therapy, created the concept of the polyvagal ladder as a visual metaphor for how we experience physiological change as we move through the three neural circuits of the autonomic nervous system.
Ventral Vagus
At the top of the ladder is the ventral vagus, where the feelings are likely to be safety, comfort, and engagement in the world around you. You’re generally feeling content, generally lacking in acute worry about anything.
Sympathetic
Just below the ventral vagus on the ladder is the sympathetic state, the place you move to for mobilization if you detect risk. This could be something relatively small, like receiving a vague email request for a meeting from your boss that causes you to wonder if you’ve done something wrong, or something as frightening as hearing a window break in your house in the middle of the night and worrying that you are about to become a victim of a home invasion. In both cases, your heart may start beating faster, your palms might sweat, and your mind may race as you worry about what could happen next.
Dorsal Vagus
At the bottom of the ladder is the dorsal vagus, where shutdown occurs. In the example of the email from your boss, if it turns out you were called into the office and fired, you’d likely move down the ladder from sympathetic to dorsal state, and shutdown might look like extreme sadness or a bout of depression. In the broken window example, if it became clear quickly that you are about to be a victim of a home invasion, shutdown could involve fainting or going into shock as a way for your body to protect you from a potentially catastrophic physical confrontation.
In both instances, it’s possible to move up the polyvagal ladder instead of down, depending on the circumstance. In the example of the email, if you went to the meeting with your boss in a sympathetic state, heart racing and palms sweating, and it turns out it was a minor request about a project, you could quickly move back up the ladder into the safe and social ventral state, relieved that your fears about being fired were misplaced. And the same is true in the broken window example. If you discover it wasn’t a broken window after all, but instead a television that was left on with the volume up very loud, you would likely bounce quickly up the ladder to ventral vagus, relieved that you and your family aren’t in danger after all.
Hybrid States of the Polyvagal Ladder
There are scenarios where two of the three neural states are combined. Stanley Rosenberg, author of Accessing the Healing Power of the Vagus Nerve, calls these “hybrid states.”14 The fourth state combines the ventral vagal (safe and social) and sympathetic (mobilization) to create mobilization without fear. Examples of this might be going to a zumba class, playing tag with your kids, or engaging in a friendly competition on the basketball court with friends. The fifth state combines the ventral vagal (safe and social) with dorsal vagal (shutdown) to create immobilization without fear. This creates a feeling of calm and safety, and examples could include lying still with a trusted partner after intimacy, or cuddling with your sleepy child before bedtime.
If you’re stuck in a dorsal state and feel like you don’t have any get-up-and-go, breath can help.
How To Move Between States With Breath
Unless you’re in a hybrid state like the examples mentioned above, which includes the safe and social feelings of the ventral vagus complex, being stuck in a sympathetic (fight-or-flight) or dorsal (shutdown) state can be draining to maintain— mentally, emotionally, and physically. If you’re locked in a sympathetic state, you might feel like you’re constantly stressed, always waiting for another metaphorical shoe to drop. If you’re locked in a dorsal state, you may find yourself in a perpetual malaise, unable to meaningfully engage with the people in your life the world around you.
Luckily, there’s a readily available way to move yourself up the polyvagal ladder to include the safe and social feelings of the ventral state, and it starts with your breath. “The simplest vagal stimulation that you can recruit is being able to exhale slowly,” says Dr. Stephen Porges. Stimulating the vagus nerve with slow exhales slows down the heart rate and gives your body cues of safety. “In the brain stem there’s actually kind of like a switch,” continues Porges. “It’s like a hot water/cold water option on the same knob. When you exhale, the vagal influences to your heart’s pacemaker get optimized. When you inhale, your heart rate goes up. And when you exhale, your heart rate goes down. If you spend more of your time exhaling, you calm your body down. If you shift rations so that most of the time you’re inhaling, you’re hyperventilating. You’re huffing and puffing. When you see anxious people, they’re inhaling on virtually every sentence or every word. They’re huffing and puffing.”
Tune Up Fitness founder Jill Miller designed an entire immersion program, Breath & Bliss, around the polyvagal theory, using breath work, position, movement, community, and a soft, air-filled sponge ball to manually stimulate the vagus nerve, and give students tools to move out of a fight-or-flight or shutdown state. “I want people to feel like they have as many options as possible to be able to modulate their own state,” says Miller. “And to understand the ‘why’ really helps with the experience of it. My bias is that I believe once you know that you can shift your physiology and you train yourself to witness your physiological shifts, it becomes a richer experience and you don’t feel so victimized by your moods or reaction to things. I want empowered recovery to be in everyone’s toolkit.”
Breath & Bliss is a movement and breath-based approach that leans into Porges’s theory of how we respond to our environment, and uses that knowledge for guidance on getting ourselves to a state where we can feel safe with ourselves and in the company of others. “One attribute of being a human being is that our body reacts to threat,” says Porges. “But it doesn’t just react to threat, it transforms how we interact with other people. So we have to understand that our body is shifting states to try and take good care of us, but in doing that, it distorts how we see the world. We know that our bodies change states and promote certain attributes to protect us. The issue is, can we create the structure and context for our bodies to feel welcoming enough to bring other people into our world? Can we give up our chronic need to be defensive, to take a chance to be accessible and live with our own vulnerability?”
Senior Tune Up Fitness® Instructor Lisa Hebert leads the Breath & Bliss Immersion internationally and has seen it transform students as they learn how to move between states. “I think the beauty of the polyvagal theory is that it brings us back to basics,” says Hebert. “Social interaction, human touch, human connection, a caring voice. All of these things we know so innately when we have a baby in our arms, but we grow up and push all that away so we can get tough and do everything ourselves. So we may lose it temporarily, but it’s this innate knowledge that we have in our gut somewhere.”
Hebert has also done Breath & Bliss work with first responders and former military members with PTSD. Jason Burd was a firefighter in Canada who almost died when a roof collapsed in during a rescue operation in 2006. After the accident he went back to work, but suffered a back injury in 2010, followed by a lung injury in 2011. He ended his career as a firefighter because of physical pain, PTSD, and suicidal thoughts. He did Breath & Bliss with Hebert, where he learned breathing exercises and rolling techniques to stimulate the vagus nerve with the Coregeous ball. “There were so many lightbulb moments,” says Hurd. “I realized that my recovery is in my hands. When I came home after the first day of the course I told my wife that I felt like the inside of my neck was bigger. My ability to breathe felt completely different. Now I use the Coregeous ball a minimum of once a day, usually twice.”
Hurd’s experience is an example of how tuning in to breath, and manually stimulating your own vagus nerve, can result in a powerful shift from chronic pain and fight-or-flight anxiety, to empowered recovery.
“That is what I call embodiment,” says Miller. “It’s when someone feels their way through their body, engaging in a conscious dialogue of their senses, feelings, urges, and needs. Be willing to respond and parent yourself with curiosity and support.”
According to Dr. Porges, understanding polyvagal theory can help us negotiate with our bodies to optimize our experiences. “Amazingly, when you become more aware of what your body’s trying to do, the body tries to work with you. We’ve treated our body as if it was something that we had to contain or control. But the message is that we live in our body. Treat your body with honor and respect, and your body will serve you well.”
Of all the good news science is telling us about the vagus, perhaps the most important is that we have the ability to befriend this wandering nerve right this very minute. While researchers all over the world continue to explore ways modern medicine can use the vagus nerve to heal chronic disease, you can start breathing now. You can start listening to the cues your body is giving you now. You can begin taking your recovery into your own hands now. For more on the vagus and building resilience, see Jill Miller’s new book Body by Breath.
At-A-Glance: How to Stimulate Your Vagus Nerve to Turn ON Your OFF Switch
To help your body “turn on” the vagus to improve its function, there are several social, physiological and physical “tricks” that your body can employ.
-
- The easiest way to stimulate the vagus nerve is through slow, deep, diaphragmatic breathing that emphasizes elongation of exhales.
-
- Singing, humming, or playing a wind instrument also excite this downregulation nerve. (As demonstrated below.)
- Massaging areas of the body which are innervated by the vagus alters vagal tone and provides a relaxation response. These include tolerable pressure to:
- Muscles of face, side and front of neck and head
- Ribcage
- Abdomen
- Positioning the body in ways that compress and decompress areas where the vagus nerve innervates:
- Rocking, which gently oscillates the head
- Neck stretches
- Abdominal and torso rotations that compress and decompress the viscera
- Gently flexing and extending the spine to affect pressure and/or stretch in the visceral area
- Chewing food, sucking on food/objects and gargling
- Safely rubbing the inside of your ear (the bowl shaped bits, not your ear canal)
- Positive social interactions
- “Feeling safe in the arms of another” or “Feeling safe in the arms of another appropriate mammal, like a dog,” Dr. Stephen Porges
- Meditation and Yoga
Learn how to Turn ON Your OFF Switch!
Download our handy guide The 5 P’s of the Parasympathetic Nervous System.
Endnotes
- Stanley Rosenberg, Accessing the Healing Power of the Vagus Nerve, (California: North Atlantic Books, 2017), 37.
- Vince, Gaia. “Hacking the Nervous System to Heal the Body.” Discover Magazine, May 2015
- Breit, Sigrid, et al. ‘Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders’, Frontiers in Psychiatry, 13 March 2018.
- Tracey, Kevin J., “The Inflammatory Reflex,” Nature, 19 December 2002.
- “How Electricity Could Replace Your Medications.” YouTube, uploaded by TEDMED, 26 May 2016.
- Koopman, Frieda A., et al. ‘Vagus Nerve Stimulates Cytokine Production and Attenuates Disease Severity in Rheumatoid Arthritis’, Proceedings of the National Academy of Sciences of the United States of America, 19 July 2016.
- Porges, Stephen, “The Pocket Guide to the Polyvagal Theory,” (New York: W. W. Norton & Company, Inc., 2017), 15.
- Stanley Rosenberg, Accessing the Healing Power of the Vagus Nerve, (California: North Atlantic Books, 2017), 19.
- Stanley Rosenberg, Accessing the Healing Power of the Vagus Nerve, (California: North Atlantic Books, 2017), 32.
- IMAIOS e-Anatomy online,
- Dana, Deb, “The Polyvagal Theory in Therapy,” (New York: W.W. Norton & Company, Inc., 2018), 4.
- Scudallari, Megan, “Scientists Discover How Vagus Nerve Stimulation Treats Rheumatoid Arthritis,” IEEE Spectrum, 18 July 2016.
- Porges, Stephen, “The Pocket Guide to the Polyvagal Theory,” (New York: W. W. Norton & Company, Inc., 2017), 9.
- Stanley Rosenberg, Accessing the Healing Power of the Vagus Nerve, (California: North Atlantic Books, 2017), 33.

















Thank you for a great blog post that sparked some really insightful comments. I especially loved the metaphors you used to explain the functions of the Vagus nerve—they’re easy to understand and relatable, which will make it easier for me to share with my students. Lisa Hebert’s thoughts on the beauty of polyvagal theory, especially the idea that it “brings us back to basics,” really got me thinking about longevity again. The Blue Zones theory suggests that people in these areas live longer, healthier lives because of factors like strong social connections, plant-based diets, regular exercise, a sense of purpose, and a low-stress lifestyle. But the biggest factor, I think, is what Lisa points out about the Vagus nerve: “Social interaction, human touch, human connection, a caring voice.” It reminded me of last week, when I was feeling stressed and reached out to a friend. Just meeting and talking about my issue, even without finding a solution, made me feel so much better.
Ahhhh the wanderer. This article is a very thorough intro to vagus theory and down-regulation practice. “Turn ON your OFF switch.” = Genius. Deb Dana’s concept of the polyvagal ladder really resonates for me. Pretty sure I heard her say one time that the pursuit is not to stay in ventral vagal, but to be nimble in climbing up and down all of the rungs. And surely, we spend much of our time in hybrid states. After some months of playing with an exercise in Rosenburg’s book which utilizes eye movements to access the upper fibers of the vagus and its passage at C1 & C2, I began to experience some wild yawns where I feel the fascias of the back of my throat unwinding in a very distinct way. This is particular swizzle-yawn has now carried over to being evoked by some of the other recommended explorations for down-regulation here. The body speaks. This education is peacemaking, personally and globally.
Really a thorough read and some new information I wasn’t aware of the vagus nerve such as all it’s points of innervation.
In my occupational therapy practice, I apply and use concepts the polyvagal theory daily. Adding to the co-regulation aspect, is our mirror neurons, which I find useful when working with young ones that don’t always comprehend our instructions with breathing and doing all these poses. You may have also experienced this yourself as your watching the videos and feel a sense of calm. My three go to activities involve deep pressure, sucking and rythmic movements which allows the child in distress to melt.
This article does an excellent job of breaking down the complexities of the vagus nerve and the Polyvagal Theory. I hadn’t considered the importance of manual stimulation to the vagus nerve before now. I gained a better understanding of how massage promotes well-being. It is interesting that vocalizing and singing also promote a ventral vagal state. The Five P’s of the Parasympathetic Nervous System is a relatable and simple guide to promoting a ventral vagal state. We can’t control what goes on around us, inner relaxation and peace really is found by looking within.
Studying anatomy can be so exciting, but also frustrating because we learn about the body by compartmentalization of the whole. I have learned and relearned different aspects of our body separately and then piece it back. This article has helped me to not only understand the physical path of the Vagus nerve, but I can get a better grip on the body as a whole and all its contributions. What really stands out is how the breath can be a tool with the tune up balls. The longer the exhale, the more relaxation and less anxiety involved. This is a great help to do bodywork and remember grounding techniques with breath as we push into the muscles and fascia. It is truly alll connected!
This is an amazingly researched and very straight forward presentation for anyone wanting to learn more about the vagus nerve. I’ve walked away with a new podcast to listen to and a linked article to learn more about how the Roman Empire was interested in it. I’m also excited to learn more about how electronic vagus nerve stimulation will make its way into modern medicine as a (likely) much more effective treatment than some medications!
Thank you for this thorough article on the vagus nerve and different ways to activate it. I was aware that it was stimulated by the breath, particularly a prolonged exhale. However, I have patients who have anxiety and have difficulty relaxing when they breathe. I appreciate that you provided examples of other ways to induce a relaxation response ex facial massage. I am wondering how effective these methods are to a skeptic. Do people have to “buy in” to the theory for it to be effective? Also are there ways of targeting the neck or abdomen without the use of a coregeous ball?
This post was a great primer on polyvagal theory and I wonder about the increasing controversy around claims regarding how to stimulate, and the effects of stimulating, the vagal nerves. For my own education, I look forward to reading more on the findings from diverse researchers on the functions of this wandering nerve.
This article beautifully captures the profound impact of the vagus nerve and its role in regulating our nervous system. Since discovering polyvagal theory, incorporating nervous system regulation into my yoga classes has become one of my key objectives. The understanding that we can consciously influence our state of being through simple techniques is truly transformative.
One aspect that has particularly resonated with me is the use of sound in self-massage and breathwork as a way to stimulate the vagus nerve. The idea that something as accessible as humming, chanting, or playing a wind instrument can have such a calming effect on our bodies is both beautiful and empowering. I’ve found that incorporating these sound techniques into my yoga practice not only enhances relaxation but also deepens the connection between mind and body. It’s a gentle yet powerful way to help my students transition from a state of stress or agitation to one of calm and safety.
The polyvagal theory, with its focus on the different states of the nervous system and how we can move between them, has given me a new framework for understanding how to create a safe and supportive environment in my classes. By integrating techniques that stimulate the vagus nerve, I can help my students not only achieve physical relaxation but also cultivate a sense of emotional and psychological well-being.
The article’s emphasis on the accessibility of vagus nerve stimulation is also deeply encouraging. The fact that we don’t need complex equipment or invasive procedures to tap into the healing power of the vagus nerve is a reminder of how capable our bodies are of self-regulation. Simple practices like breathwork, gentle movement, and even positive social interactions can have a profound impact on our overall health.
Thank you for shedding light on the importance of the vagus nerve and how we can harness its potential for our well-being. This article is a wonderful resource for anyone looking to deepen their understanding of the mind-body connection and find practical ways to enhance their self-care routine.
I can’t express enough how grateful I am for this article. Although a lot of the information I have come across through other means it was very nice to get a refresh and get a deeper visual picture of this massive “wondering” nerve. The techniques have inspired a how series of restorative classes I’m excited to bring to my students. I can’t wait for the day when I can articulated the different areas and zone of palpation like Jill. I’d love to help inform my students on their anatomy in that way. Till then I’ll just have to simplify the terminology a bit.
This article is very well written, clearly and digestibly sharing the components of Polyvagal theory. I appreciate the inclusion of the videos to try for switching into the ventral state. I am so glad this is one I chose to read. I teach Stress Management at a University and I am looking forward to including this as a resource as well as further delving into the resources cited in the article.
Thank you so much for this blog post. I was somewhat familiar with polyvagal theory, but this article presents it in a clear and concise, yet thorough manner. Some of the techniques to stimulate the vagus nerve were familiar, and others were new to me. I’m looking forward to using the tapping technique next time I need to energize, and I’m also excited to incorporate the downregulating techniques with students prior to savasana. I’ll also be on the lookout for the next Body by Breath immersion – I just purchased the book and can’t wait to delve into that as well.
I really appreciated the mention of hybrid polyvagal states. It can be really easy to generalize sympathetic or dorsal vagal states as broadly undesirable, but this was a great reminder that, when combined with the ventral vagal state, these are some of the best moments in life! Hadn’t encountered the tapping for mobilization before– looking forward to using this practice the next time I need a pick-me-up.
Great article! Love the variety of options to stimulate the vagus nerve making it accessible for folks. I have done vagal work with chanting and breathwork in yoga, and am excited to incorporate more techniques.
This is my favorite article on the blog so far! I’m about five years into polyvagal theory and it completely transformed my understanding of myself and the concept OPTIONS when it comes to modulating physiological states and the energy, mood, emotion, and sensations that come with them. I completely agree with Jill that once we know and trust that we can modulate our states – and spend time practicing those skills – it completely transforms the experience of being inside one’s body. This paradigm shifting framework helps me nurture an intimate relationship with my nervous system that centers agency, trust and respect. The tapping video was new to me and it gave me a lovely boost! And the visceral massage is my number one morning go to – it sounds strange to say so but it feels like a sacred practice and it is surely the access to the vagus nerve and what we can reflect/digest/integrate in down regulated states that feels so profound.
Since opening my YTU certification manual last week I have renewed my interest in my breathe and the effect it has on my state of mind. Work has been really stressful for the past couple of weeks, so the breath section like a real gift from the universe. This article provided even more great information and I am looking forward to using many of the techniques, both with myself and in yoga/pilates classes that I teach. For now, I have just been focusing on downregulating my emotional state through concentrating on breathing with longer exhalations than inhalations. It is so simple, but the effect on the vagus nerve is tremendous. I am doing this at bed time, and am enjoying being able to get to sleep much more quickly.
Thank you for this article! I recently completed the amazing Body by Breath Immersion and we learned about the Vagus Nerve in depth, and it is so helpful to continue to learn and experience it. In my own practice, I LOVE using the Corgeous ball to palpate my neck muscles, especially my sternocleidomastoids and scalenes.I admit that before the immersion I was inclined to use the Tune Up balls on these muscles, but we learned that less can be more especially when it comes to the neck. The Corgeous Ball has also been an amazing tool for me in Zones 1 and 2. II’ve always had trouble with deeper breathing and having the feedback from the ball as I breath has been a game changer. I have been using it with private clients ,and I recently using it in my first workshop with the balls! Like me, I think people are wary of what the Corgeous ball can do at first and want to go straight to the “hard stuff”, but then they experience how great it is. I have also been getting great feedback on the square breath; I have been using the 4-4-6-4 pattern.
This was such a perfect blog to read after the one on the diaphragm. And it’s really amazing the potential that this work with the vagus nerve has for those with PTSD. I also had no idea how extensive this nerve is and how far its reach is!
I’ve studied the vagus nerve and am familiar with polyvagal theory where I was introduced to this through the book “the Body Keeps the Score.” I knew about the connection to the vagus nerve through the breath, but have not considered massage and using these techniques for PTSD. I also was not aware of the anatomical connections with the vagus nerve and its vast role in physiology.
Thank you for the in depth information on the Vagus nerve. As knowledge about (and as people are learning of) the vagus nerve, it is assuring to have simple tools that everyone can access (the prolonged exhale).
Wow! What a thorough journey sailing into the depths of the vagus nerve. I tried out all of the accompanying video practices and I’m feeling quite serene having experienced them all. Even if you don’t have the balls, which I highly recommend, you can use your breath to calm your nervous system. The vagus nerve is our internal caretaker and can settle us in moments. Our bodies are incredible.
I loved this article for explaining how and why the vagus nerve is so influential to our body’s health, and for showing so many ways that a person can take vagus nerve balance into his or her own hands. I especially love the neck massage with the Coregeous ball and the sounding exercise.
Very informative and helpful article on the Vagus Nerve. I loved the “Vagus Nerve: Tapping to Mobilize” video for increasing your energy when “you’re stuck in a dorsal state and feel like you don’t have any get-up-and-go”.
Very informative article. It gives a good overview of current research and clear instructions on how to stimulate the nerve.
I’ve been learning so much about the vagus nerve lately and the impact it has. I like the part that highlights how even dorsal activation isn’t a bad thing, say when paired with parasympathetic states like cuddling. It’s so important to know how to work with this part of ourselves because if we are in shutdown for extended periods like I was growing up, then anything we do is like trying to drive the car on the freeway with the emergency brake on. Eventually it’s going to shudder and break down!
The Vagus nerve has to be the most complex and fascinating of all craneal nerves. With all the inervations through so many areas and organs in the body it creates a network to inform our brain (80% of the messages are afferent, to the brain) of our connections with our outer world (friendly or foe) and how we need to respond to survive and be safe. It’s a basic survival response that we evolved way back before our complex rational thought processing in the frontal cortex. What blows my mind is that such a basic function can be modulated consciously with our breath, through the inervations in the diaphragm, to slow down the heart rate and inform the brain that we are safe. This is literally the bridge between the unconscious and conscious mind. This is what makes us human.
I have done this class, Amazing! changed the sound of my voice!
helpful article to have the info and videos together THANK YOU
I recently listened to the audible book “Breath” by James Nestor, and I find this article to be just as useful. I really love how the Vagus Nerve can be manipulated for upward, or downward regulation, and we are able to navigate our autonomic nervous system through the Vagus Nerve. Absolutely- incredible!
Thank you for an informative article on the amazing vagus nerve. I was interested to learn that vagal stimulation decreased TNF-alpha in people with rheumatoid arthritis AND that the breath is an easy doorway in to vagal activation (prolonged exhalations) … should everyone be taking breathing breaks to promote their optimal health? I look forward to reading more about Dr. Kevin Tracey’s research.
It’s beautiful the way that the vagus nerve can be accessed, bridging numerous professions and that we all can make a difference with the people we work with, using this knowledge. Hearing about how Gregg Johnson experienced the manual palpation of the vagus nerve on one of his students helped illustrate to me that tension can be held there specifically and cause health issues, and that wasn’t something that I understood before, although I had understood that palpation or use of the therapy balls on vagus nerve output areas all over the body could be helpful. So that makes a lot of sense! I love learning more here about the various health challenges that can be amerliorated via vagus nerve stimulation (VNS), and had heard about epilepsy and other medically intractable seizure treatment trials with VNS in the past. I also love hearing about the polyvagal podcast and the vagus study group, and knowing that an LMFT started the former, and also that Deb Dana is an LCSW, which leads me to believe I will be able to incorporate this work into my eventual clinical social work, which is inspiring. I just think about how interesting neuroanatomy courses would be if they made sure to go more into depth about the vagus nerve, learning about the current clinical application on VNS addition to its relationship to other cranial nerves. So much to say and respond to here! Great article and compilation of resources that I’ll return to.
The woodcut of cranial nerves you display on this site was done in 1537 by Andreas Vaselius, a 16thC physician. It is of all 12 cranial nerves including the vagus which is number X. If you look more closely at the drawing you will see the nerves are indicated by numbers. This drawing was based mostly on animal studies and notes from the works of Galen of Pergamon, an ancient Greek physician who had been dead for 1,300 years before it was created. The vagus does not descend to the groin nor the descending colon – that should have been a clue. For more information, go to https://www.cambridge.org/ and look for the article entitled, THE ORIGINS OF THE SYMPATHETIC NERVOUS SYSTEM FROM VESALIUS TO RIOLAN by Roger French, p. 47-48. It explains the origin of the woodcut as well as it’s numerous errors.
****************
La gravure sur bois des nerfs crâniens que vous présentez sur ce site a été réalisée en 1537 par Andreas Vaselius, un médecin du XVIe siècle. Elle représente les 12 nerfs crâniens, y compris le nerf vague qui porte le numéro X. Si vous regardez le dessin de plus près, vous verrez que les nerfs sont indiqués par des numéros. Ce dessin a été réalisé principalement à partir d’études sur des animaux et de notes tirées des travaux de Galien de Pergame, un médecin de la Grèce antique décédé 1 300 ans avant sa création. Le nerf vague ne descend pas jusqu’à l’aine ni jusqu’au côlon descendant – cela aurait dû être un indice. Pour plus d’informations, rendez-vous sur le site https://www.cambridge.org/ et recherchez l’article intitulé “LES ORIGINES DU SYSTÈME NERVEUX SYMPATHETIQUE DU VESALIUS AU RIOLAN” par Roger French, p. 47-48. Il explique l’origine de la gravure sur bois ainsi que ses nombreuses erreurs.
« Nous avons traité notre corps comme si c’était quelque chose que nous devions contenir ou contrôler. Traitez votre corps avec honneur et respect, et votre corps vous servira bien ». Cette phrase raisonne tellement en moi, j’ai adoré lire cet article et je n’ai qu’une envie c’est de continuer à en apprendre encore plus sur ce nerf si puissant. Ma prochaine lecture va être le livre de Stephen Porgues
Je prends conscience de la puissance du nerf vague, c’est incroyable ! J’adore,
je vais le chouchouter !
“La puissance du nerf vague réside dans sa capacité à avoir un impact sur les
conditions physiques et émotionnelles qui se sont avérées difficiles à traiter avec
des médicaments traditionnels et des interventions médicales. Lorsque les gens
sont à court d’options – pour les troubles médicaux ou la gestion du stress – ils
trouvent leur chemin vers le vide et réalisent le pouvoir que cette partie de notre
anatomie a sur l’ensemble du système”.
Wow! Quelle découverte que je viens de faire. Ce nerf vague mérite qu’on s’en occupe en lui portant de l’attention… être aux petits soins avec lui, car il est lié à l’humeur, à la force de notre système immunitaire, à notre digestion et à notre fréquence cardiaque.
Je sors mes balles et j’ajoute ce massage à cette partie de mon corps. Le nerf vague…mon nouvel ami…À ne pas négliger!
Article très intéressant avec une explication simple et claire sur le fonctionnement du nerf vague. ça donne envie d’aller plus loin sur le sujet. merci
Wow: “The vagus has more than 100,000 nerve fibers, and communicates bidirectionally between the brain and the body, with 80% of the fibers communicating from the body to the brain, and the other 20% communicating from the brain to the body.12 So, that “gut feeling” you’ve felt before— that’s neuroception. It’s your body having what amounts to a “sixth sense” moment, and communicating that information to your brain.” Thank you for that article!
Very interesting,I really like this article !
Vagus Nerve has a major impact on the whole balance of the body. Having already practiced these exercises with coregeous ball, I can say that the results are amazing.
C’est de façon sûre mon prochain sujet d’étude ! J’ai déjà acheté un livre pour en connaître davantage.
Thank you for this very thorough overview. I love the hands on Roll Method approach, the 5 P’s and the neuroscience background. Thank you for bringing all this information to our fingertips and minds in such a organized and easy to understand format.
I LOVED this article so much! It was so informative and eye opening especially with the photos and videos.
This is an article every human should read!
I especially LOVE this metaphor “ A symphony conductor, directing how fast or slow, loud or quiet your nervous system will be at any given time” it paints such a vivid picture of the vagus nerve and it’s Important role in our body
Love the variety of techniques and ways to tune into the each of the three neural circuits of the polyvagal ladder. I find it incredible how we can manipulate our nervous system in these simple ways.
Fertility Treatment
Best treatment for female and male infertility issues!
Thank you for empowering us not only with knowledge about Vagus nerve but also with its applications into many real life techniques to stimulate relaxation response. 5 Ps for the win!
Wow. This is my first time reading about the vagus nerve and I can’t wait to try these coregeous breath work exercises. I often sway side to side as I stand and now I see that’s my body’s way of trying to calm some of my anxiety. Can’t wait to read more!
This is a wonderful and easy to follow introduction to the functions of the vagus nerve complex. I especially enjoyed looking further into the bioelectric movement of vagal nerve stimulation as it relates to treatment for digestive disorders and Parkinson’s. The very clear videos and steps to help us all create awareness of and tone within our vagal nerve responses was amazing! I love the rib cage and abdominal rolling on the coregeous ball but I never thought to do the same for my neck area of the vagus nerve. Thank you!
The Vagus and The Coregeous Ball go hand in hand!! All such good tips for learning how to connect better in the body!
I’m hearing much discussion about the vagus nerve and it’s abilities for regulating. In the section, co-regulating, I am interested to know if the co-regulation can be reversed-baby cries, mother tries but unable to sooth and becomes upset creating more upset. Everyone is upset, now if mother can relax (breath, meditate) will/can baby then take on that emotion?
I was happy to find the section of the blog on use of the gorgeous ball for stimulating the vagus nerve for relaxation! It is not something I have been focusing on of late and this is encouraging me to delve deeper and experiment with my gorgeous ball! OM, OM , OM…
The most concrete idea I found in this article about deregulating the vagus nerve was that the heart rate slows when breathing out and speeds when breathing in so if you spend more time breathing out, you will feel more relaxed. Perhaps this breathing techniques also helps with sleep.
As a long time choral singer, i’ve always wondered about how singing can cause the feeling of well being and peace, particularly with slow, melodic, simple music. After reading this, I see the connection between certain kinds of singing–or chanting– and vagus stimulation. Krishna Das is stimulating the vagus nerve!
what is electronic vagus nerve stimulation? and is it more effective than self myofascial release for stimulating the vagus nerve and inducing a parasympathetic response?
I love Dr Porges reminder that our body is not something that we must control but rather something to work with. It is so true that we often fight what our body wants or what it is trying to tell us but if we listen more or tune into it we may find the answers sooner than if we were to just plow through. The ladder was also helpful in understanding the depth of involvement if the vagus nerve. Fascinating stuff!
I would like to hear more…
Interested?
Thanks for sharing.
Thank you
Thanks for sharing . Where. Purchase the balls?
This was such a helpful and informative synopsis of the vagus nerve. I knew the vagus was a hot topic and had a vague (ha!) idea of its connection to the parasympathetic response and relaxation, but this really helped me to understand how and why that is the case. I can’t wait to dive into those practice videos for myself tomorrow – simply watching them was already relaxing! Consider my interest totally piqued in learning more about the body’s “off switch”.
I really like this article on the Vagus Nerve … it is clear, comprehensive, and accompanied by appropriate exercise. This fascinating text to read does justice to the symphonic conductor who is the 10th cranial nerve directing our nervous system which will be fast or slow, strong or silent depending on the moment. We can, with this polyvagal theory, look with new eyes at our way of thinking and living our body and our beings, our emotions and our interaction with the environment!
thank you.
I agree that lengthening the exhales and humming (bumblebee breath) have been very helpful in bringing on the relaxation response.
Hi… I’m very interested.
I am a bit concerned that this article doesn’t mention the health care partnership required to achieve total health and wellbeing. Those with an overactivated sympathetic nervous system may also require the help of mental health professionals to avoid retraumatization through a physical practice. “Overcoming Trauma through Yoga: Reclaiming Your Body” developed at the Trauma Center at Justice Resource Institute does state that the use of props (including therapy balls) can be triggering. How would you react if someone started crying or became violent in your class? There is definitely a need for trauma-sensitive yoga and roll models. This is really an ongoing partnership from my perspective.
Learning the palpation and vagal nerve manipulation tools suggested here is helpful as an addition to my current understanding and breathwork practise of this intricate system. I look forward to using the tune up balls to assist down regulation of my nervous system then to offer and guide clients in the future
I am looking forward to my next apt. with my PCP…
Great practical info you sharing, thanx!
im a massage therapist and interested in keeping up with all the great blogs you provide.
That’s a new concept to me. Thanks for sharing it in such detail. Will try the exercises for positive results.
Thanks!
Thank you so much for presenting all the exercises to stimulate your vagus-nerve and all the details scientific theories!!
Vegus nerve stimulation exercises
I have vasovagal syncope. Basically, when my vagal system is innervated, my blood vessels dilate, blood leaves my brain, and I pass out. It’s much worse than just that, but that’s basically what happens. Do you know if any of your exercises/maneuvers might help to strengthen my vagus nerve, or will these trigger me? I am desperate for something that will prevent these attacks. Interestingly, I also have Crohn’s disease, which you mention as being related to the vagus nerve.
Thanks for any help.
Thanks Suzanne. I didn’t know that the vagus nerve had three parts (ventral- safe and secure, sympathetic, fight or flight, and dorsal, shutdown) with the possibility to combine them to optimize sport or deep relaxation. I can’t wait to try some of these techniques to stimulate my vagus nerve!
Discovery of the day. I am breathtaking and wish to learn more.
I will try the massage prior to going to sleep.
There is a lot to learn on the vagus nerve … I will have to watch all the videos!
This part of the article (Hurd’s experience is an example of how tuning in to breath, and manually stimulating your own vagus nerve, can result in a powerful shift from chronic pain and fight-or-flight anxiety, to empowered recovery.) is very important! Everybody, with knowledge, can enhance his ou her health! Thank you. The video of self-massage of the facial fascia will be very helpful.
I have been wondering about the vagal nerve for a while. I know it matters, but I hadnt yet taken the time to learn about its role and its impact on our daily lives. I really liked the exercices. I could feel a great physical and mental ease. I felt relaxed and more grounded. I will share this article to clients and friends.
It is always so interesting to read about the vagus nerve. It is very complex, but it it is worth taking the time to understand. I will also definetly read again the ”At-A-Glance: How to Stimulate Your Vagus Nerve to Turn ON Your OFF Switch” section!
C’est réellement intéressant. Je me rend compte de plus en plus de l’importance du nerf vague sur mon système de “gestion du stress” . Il est stimulé à la parole et durant la covide le nombres de mots dans une journées est passé de extrêmes à pratiquement rien, j’ai alors perçu un manque de stimulation. Habituellement pour me rendre au travail je chante dans l’auto et mes 2 travail exigent beaucoup de communication avec les gens. Je me suis donc mise à écouter de la musique en jardinant et je chantais. J’ai rapidement observé un état mentale moins descendant et une relaxation plus facile.
Super intéressant,
je découvre l’impact majeur qu’a le nerd vaque sur l’ensemble de l’équilibre du corps. De plus , l’étendu de ses ramifications et la perspective de pouvoir le stimuler pour apaiser ou équilibrer des organes internes ou émotionnelles qui en auraient besoin.
Love your work!
Very informative.
Thanks for this talk on the Vagus Nerve!
Helpful ideas needed to help clients and personal need to balance motor planning center and lymphatic system. Thanks for any ideas that can be shared. Been working with the polyvagal nerves for over four plus years to help trauma victims and multiple years working with sexual abuse victims.
Encephalitis of both temporal lobes/hippocampus of my brain left me with amnesia, seizures, dementia issues, and a nonstop state of Depersonalization and Derealization. I was installed with a Vagus Nerve Stimulator for seizure control. Turns out not only does stimulating my Vagus nerve stop my seizures on the spot. Well it also has made it possible to feel emotions and connections to life and people in it again. Our vagus nerve is where our love, empathy, and passion comes from. Also stimulating my Vagus nerve assists in weight loss. Since our vagus nerve goes through our thyroid. Then when activated it is speeding up my digestive system. Since this nerve goes through our stomachs. Then when activated it is telling my stomach I am full. So it curbs my appetite. I could continue as well. Science is discovering our vagus nerve is our bodie’s natural healer.
This article is amazing. Through every video I could feel a great physical and mental ease, relaxation and grounding. We should all be aware of the vagal complex and its repercussions to our health, anxiety and changing moods, and simply to the way we see & live our life. Thanks again for this very complete article!
Thank you
Just took a Breath Course in which we learned about the Vagus Nerve. I am so interested in learning more…
thanks for this awesome info.
Thank you for the comprehensive article – it is very helpful to understanding a complex subject.
Such a great post! I can not wait to try the ribcage massage. The more I learn about the vagus nerve, the more I want to learn. Keep it coming!
This is a subject I am diving deep into! Excited to learn more. You are a fantastic teacher.
Yes! I took Breath and Bliss 3 years ago and fell in love with learning about the Vagus Nerve. It is so empowering to be able to self soothe and use your own touch to calm and bring oneself into parasympathetic state. It is most rewarding to teach others how to do the same. Thank you for your article!
Thank you very much for this generous and very complete text and exercises. Wow!
It is important to disseminate this information to as many people as possible.